- Jennifer Roberts
Choose the health content that’s right for you, and get it delivered right in your inbox.

It was a Monday similar to so many others in Hollie Mahadeo’s life. She had worked from home, picked up her seven-year-old son from the school bus stop, and returned home to get a little more work done before calling it a day.
But Mahadeo never made it back to her desk.
As she climbed the stairs to her home office, her legs suddenly felt heavier than usual. As she reached the top, she dropped the glass of water she was carrying – spilling liquid and ice all over the floor.
“I remember thinking, how can I be so clumsy,” said Mahadeo. “I called to my son to come help me pick up the ice cubes, and the words came out all jumbled. I sat on the floor against the couch; my son rubbed my back and asked me to get up. But with every fiber of my will, I could not get up. All of a sudden, it clicked – I might be having a stroke.”
Mahadeo’s son ran to find her husband to help. Those minutes were critical, and they did exactly the right thing. Holly’s husband called 911 for an ambulance to come their Lake Mary home.
“The ambulance got there fast,” Mahadeo recalls later. “We went straight to AdventHealth Orlando ER.”
When Mahadeo and the EMS team arrived at the hospital, the team was ready. An ER doctor was in the room, a telehealth neurologist was dialed in and on camera, the imaging team was standing by, and the CT scanner was available; nurses were ready to take blood and administer a shot of Tissue Plasminogen Activator (tPA), the critical medication to break up a clot in the brain during a stroke.
Eighteen minutes after Mahadeo was wheeled into the AdventHealth Orlando ER, she had been evaluated by a team of experts, had a CT scan, confirmed the diagnosis was a stroke, and was given the tPA injection.
“We call it door-to-needle time,” explains Dr. Indrani Acosta, vascular neurologist and stroke medical director at AdventHealth’s Central Florida Division. “It’s the time it takes the team from when the patient arrives until tPA is administered. At AdventHealth, our goal is to treat 50% of the patients in the first 30 minutes. Time is brain. The faster we can treat a patient, the faster we can reduce the clot and get blood flowing. Hollie’s time was very fast, and she had an excellent result.”
“Before they rolled me back to a second CT scan, I was regaining my motor function,” said Mahadeo. “It was incredible the treatment worked so quickly. I was able to speak again. You wouldn’t even know I had a stroke.”
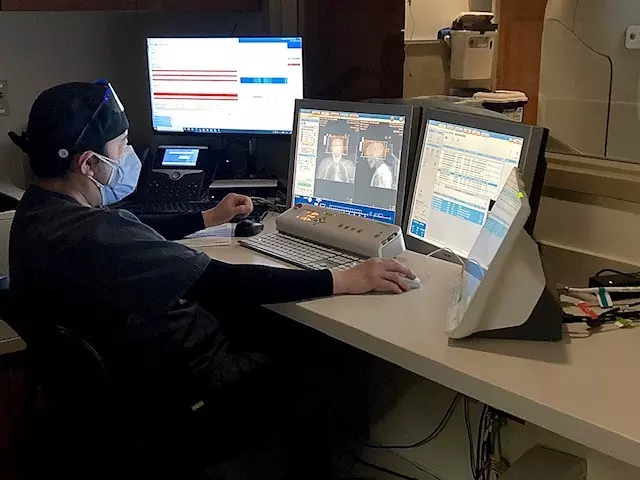
In addition to the tPA, another critical care component is the telehealth neurologist. Having that expert evaluation ready before the patient even arrives at the hospital is critical to making the right decisions quickly.
“Stroke is the leading cause of disability in the United States,” says Acosta. “But we have a shortage of neurologists. We don’t have enough people to be on call in our emergency rooms to make these life-saving diagnoses. At AdventHealth, we have neurologists on call in person, and we supplement that with telemedicine. Patients with acute stroke symptoms can be easily examined on camera. It works very well and quickly.”
The telehealth neurologists can evaluate the patient remotely and also be taken into the CT scans with them. The neurologist can observe the patient during the scan and review the results of the scan immediately.
Access to advanced neurological care in the ER and hospital is critical for providing life-saving stroke care. Quick, accurate decision-making and information provided by the Longwood Fire/Rescue team who took Mahadeo to the hospital significantly improved Holly’s chances of survival and complete recovery.
“The ambulance gives us a pre-notification of the patient coming in,” said Acosta. “When we get good information such as specific symptoms, how long the patient has experienced symptoms, and when they expect to arrive, we can prepare.”
Months after her recovery, the AdventHealth stroke team arranged for Mahadeo and her son to meet with the firefighters who helped save her life that day. The AdventHealth stroke task force members attended not only to recognize and commend the team for their rapid response but also, to provide some additional stroke education about decision making in those critical minutes before arriving at the hospital.
Just 48 hours after having a stroke, Mahadeo was discharged from the hospital and went home. Months later, thanks to quick action and access to advanced stroke care, Mahadeo had no adverse side effects of her stroke. It also alerted her to an undiagnosed heart condition – atrial fibrillation – or irregular heartbeat. It could have been the cause of the stroke. Now she is paying more attention to healthy eating, exercise, and limiting caffeine.
“In a lot of ways, I’m better than ever health-wise,” Mahadeo said.
Recent News
The Inspiring Wholeness podcast explains how to start an exercise routine, stay motivated and build endurance safely, to find your inner Ironman.
As the world rang in 2025, AdventHealth for Women welcomed the very first babies of the new year.
Dr. Joseph Lopez, chief of pediatric head and neck surgery at AdventHealth for Children, was honored with the prestigious Professional of the Year Award at the 27th Annual Don Quijote Awards.
Giving back to his hometown, Dr. Ryan Day brings advanced robotic surgery to local patients, offering life-saving care close to home.
The holiday season can increase heart attack risks due to overindulgence, stress, and ignored symptoms, but Dr. Hector Lozano advises moderation, staying active, managing stress, and sticking to...
Transplant is AdventHealth Transplant Institute’s 5000th kidney transplant
Deputies from local fire and police departments dressed as elves and dropped in to visit patients as part of an eight-year long tradition bringing festive cheer to kids and families staying at the...
AdventHealth is now using a fluorescent dye that lights up cancer cells during surgery, which is providing faster, more accurate treatment for patients.
On the newest Inspiring Wholeness podcast, Obie Diaz, local morning radio show host, shares how a routine physical eventually led to two open heart surgeries.
Inspired to change statistics around Black maternal deaths, AdventHealth for Women's Fourth Trimester Program offers enhanced postpartum care for Black mothers with high blood pressure.
AdventHealth University and Jobs Partnership Build Health Care Workforce Pipeline from Underserved Communities.
New LifeWorks Program provides health care workforce training to under-skilled job seekers throughout Central Florida.











