Location Details
AdventHealth Medical Group Orthopedics and Spine at Inverness
To request an appointment with our team, please call us at Call303-699-7325.
About Our Practice
At AdventHealth Medical Group Orthopedics and Spine at Inverness, our highly skilled orthopedic doctors and spine surgeons are committed to providing the best care for your unique needs. We’re honored to care for our South Denver community and surrounding areas.
We offer non-surgical and surgical treatment options for the spine, hand, wrist, shoulder, elbow, foot and ankle. Know that our physicians have completed fellowships in orthopedics, meaning they have comprehensive training beyond residency. We’re dedicated to learning about the latest breakthroughs in orthopedics and spine.
We care for various conditions, from broken bones and arthritis to total joint replacements, and our spine surgeons focus on delivering superb evidence-based care, including sports medicine, joint replacement, physical medicine and rehabilitation.
Surgical Options Tailored to Your Condition
Our joints are connected to our bones with tissue called cartilage. Healthy cartilage serves as the bone’s protective cushion, allowing joints to move smoothly and with low amounts of friction. If the cartilage becomes damaged by disease or injury, the tissues around the joint become inflamed, triggering pain. Over time, the cartilage wears away, allowing the rough edges of the bone to rub together, causing increased pain.
If only part of the joint is damaged, a surgeon may be able to repair or replace just the affected areas. But if the entire joint is damaged, a total joint replacement is required. To replace a total hip or knee joint, a surgeon removes the diseased or damaged parts and inserts artificial parts, called prostheses or implants.
Joint replacement procedures we offer include:
- Anterior-approach hip replacement
- Minimally invasive knee replacement
- Computer-assisted hip and knee joint replacement
- Total knee replacement (TKR)
- Unicondylar (unicompartmental) knee replacement
- Knee replacement revisions
- Hip replacement revisions
- Shoulder joint replacement
Arthroscopy is a minimally invasive surgical procedure in which an instrument called an arthroscope is inserted into the joint so that it may be inspected or worked on. Arthroscopy comes from the Greek words arthro (joint) and skopein (to examine).
The benefits of arthroscopy involve smaller incisions, faster healing and less scarring. Arthroscopic surgical procedures are often performed on an outpatient basis, and patients typically go home on the same day.
Arthroscopy procedures we perform include:
- Knee arthroscopy
- Shoulder arthroscopy
- Rotator cuff tear repairs
- Shoulder impingement repair
- ACL reconstruction
- Hip arthroscopy
Our Expert Team, Dedicated to You

Mark Fitzgerald, MD
Sports Medicine and Arthroscopy

Robert Greenhow, MD, FRCSC
Sports Medicine and Joint Specialist

Craig Loucks, MD, FRCSC
Hip and Knee Surgeon

Hugh McPherson, MD
Orthopedic Surgery, Spine Surgery

John Sharp, DPM, FACFAS, ABFAS
Foot and Ankle Surgeon

In Sok Yi, MD
Hand Surgeon
Comprehensive Spine and Joint Services
We provide expert, compassionate care for joint conditions and back pain, working to uncover the cause of your pain through imaging and diagnostic procedures. We’ll explore non-surgical treatments first, and if surgery is required, our doctors offer the latest surgical orthopedic and spine techniques, including same-day joint replacements and minimally invasive procedures.
- Anterior Approach Total Hip Replacement
-
A total hip replacement using the minimally invasive direct anterior approach is an alternative to a conventional hip replacement. Hip replacements are historically performed using posterior (back) or lateral approaches, which require making incisions into certain muscles or tendons to access the hip joint.
The direct anterior approach utilizes a muscle in front of the hip joint and doesn’t require muscles and tendons to be opened to access the joint.
Patients who have undergone a hip replacement using the anterior approach typically experience less postoperative pain and discomfort and faster recoveries. Most patients are discharged from the hospital after two days and no longer need walking aids like a cane or crutches within two weeks of surgery.
The anterior approach is not recommended for all patients. Most patients undergoing a hip arthroplasty revision benefit more from traditional methods. Patients who have hip deformities from childhood also, on occasion, are not candidates for the direct anterior approach.
- Advanced Anatomic Repair Shoulder Arthroscopy
-
The advanced anatomic repair technique for rotator cuff and labral tendon repairs utilizes multiple row or footprint attachments for tendons instead of the standard single row, allowing the surgeon to mimic anatomic tendon positioning better. This technique enables the surgeon to inspect the integrity of the shoulder anatomy better.
- Spinal Disk Replacements
-
Lumbar Artificial Disk Replacements
Lumbar artificial disk replacement is a surgical method of replacing diseased or damaged intervertebral disks with artificial disks to restore motion to the spine. It’s an alternative to spinal fusion for patients with lower back pain. It’s also an option for patients with degenerative disk disease, a gradual degeneration of the disks between the vertebrae caused by aging.
Your doctor may recommend diagnostic tests like magnetic resonance imaging (MRI), discography, computed tomography (CT scan) or X-rays to identify the cause of your pain. Patients with back pain caused by bulged or worn-out intervertebral disks and patients with no significant facet joint disease are candidates for artificial disk replacement. The surgery is not recommended for patients with scoliosis, previous spinal surgery or who are morbidly obese.
During surgery, an incision is made in the abdomen, and the muscles and the blood vessels are gently moved for a better view and room for surgery. The disk space is opened, the damaged disk is removed and replaced with the artificial disk.
Disk Design
There are two types of artificial disk designs: disk nucleus replacement and total disk replacement.
With the disk nucleus replacement, only the central portion of the disk (nucleus) is removed and replaced with a mechanical device, while the outer ring of the disk is left intact. However, the disk nucleus replacement procedure is not commonly practiced and is still in the investigative stage.
In total disk replacement, the annulus and nucleus are both replaced with a mechanical device. Artificial disks are usually made up of metal, plastic or a combination of medical-grade plastic and medical-grade cobalt chromium or titanium alloy.
Rehabilitation can begin soon after the surgery. A hospital stay of about two to four days may be required. Basic exercises, including walking and stretching, may be performed during the first few weeks after surgery.
Artificial disk replacement surgery may cause certain complications, including:
- Infection
- Injury to blood vessels
- Dislodgement or breakage of the device
- Wear of the device materials
- Continued or increasing pain
- Bleeding
- Bladder problems
- Endoscopic Carpal Tunnel Repair
-
Carpal tunnel syndrome is a common condition and can be treated with minimally invasive endoscopic surgery, which involves only a few half-inch incisions and the use of an endoscope.
In endoscopic surgery, a thin, flexible tube with a camera (endoscope) is inserted into small incisions in the wrist and hand. The endoscope helps your surgeon visualize the internal structures at the wrist, avoiding the need for a large incision. Patients are usually discharged home the same day.
Your surgeon will suggest certain postoperative care for a better recovery and to avoid complications, including:
- Elevating the hand above heart level to reduce swelling
- Wearing a splint
- Ice packs to reduce swelling
- Keeping the incision clean and dry
- Physical therapy may be ordered to restore wrist strength
- Eating a healthy diet and not smoking will promote healing
Most patients do not have any complications following carpal tunnel release surgery. If complications do arise, like continued pain or infection, we will work with you to manage your symptoms effectively.
Treatment Options for Orthopedic Conditions
- Hip
-
Hip Resurfacing
Hip resurfacing, or bone conserving, replaces the acetabulum (hip socket) and resurfaces the femoral head. This means the femoral head has some or very little bone removed and replaced with the metal component. This spares the femoral canal.
Revision Hip Replacement
This option is for patients with previous hip replacements that need to be revised. This procedure varies from minor adjustments to complex procedures that replace significant amounts of bone material.
Hip Arthroscopy
Hip arthroscopy is a relatively new surgical technique that is effective for a variety of hip conditions.
Femoroacetabular Impingement (FAI)
FAI results from abnormal pressure and friction between the hip joint's ball and socket, resulting in pain and progressive hip dysfunction. When left untreated, it leads to secondary osteoarthritis of the hip.
- Knee
-
Knee Arthroscopy
The benefits of arthroscopy include smaller incisions, faster healing and less scarring. Arthroscopic surgical procedures are often performed on an outpatient basis.
Total Knee Replacement (TKR)
A total knee replacement (TKR) or total knee arthroplasty resurfaces an arthritic knee joint with artificial metal or plastic replacement parts called prostheses.
Anterior Cruciate Ligament (ACL) Reconstruction
The ACL is a strong rope-like structure running from the femur to the tibia and is a major stabilizing ligament in the knee. When this ligament tears, it doesn't heal and often leads to instability in the knee.
ACL reconstruction is a common surgical procedure, and with recent advances, it can now be performed with minimal incisions and fewer complications.
Unicondylar Knee Replacement
In this procedure, only part of the knee joint is replaced, using a smaller incision than would be used for a total knee replacement.
The knee joint is made up of the patellofemoral, medial and lateral compartments between the femur and tibia. Often, only one of these compartments wears out, typically the medial one. If your symptoms and X-ray findings indicate this, you may be a candidate for this procedure.
Revision Knee Replacement
This means that part or all of your previous knee replacement needs to be revised. This operation varies from minor adjustments to complex operations that replace significant amounts of bone.
- Shoulder
-
Rotator Cuff Tear
The rotator cuff is the group of tendons in the shoulder that provide support and enable a wider range of motion. Major injury to these tendons may result in the tearing of these tendons, called a rotator cuff tear.
Shoulder Impingement
Also called swimmer’s shoulder, tennis shoulder or rotator cuff tendinitis, shoulder impingement is inflammation of the tendons of the shoulder joint. It can be caused by car accidents, trauma or sports like tennis, baseball, swimming and weightlifting.
Shoulder Arthroscopy
Shoulder arthroscopy is a minimally invasive surgical procedure. The benefits are smaller incisions, faster healing and less scarring. Arthroscopic surgical procedures are often outpatient surgeries, and the patient can return home on the same day.
Frozen Shoulder
Frozen shoulder is when pain and inflammation in the shoulder severely restrict movement. It’s also called adhesive capsulitis and may progress to the state where it’s very difficult to move the shoulder at all.
Shoulder Joint Replacement
Shoulder joint replacements are usually done to relieve pain and when all non-operative treatments to relieve pain haven’t been effective.
- Spine
-
Treatment options for normal spine anatomy and spinal deformities include:
- Spinal fusion
- Lumbar diskectomy
- Lumbar laminectomy
- Elbow
-
We treat a variety of elbow ailments, including:
- Elbow fracture
- Elbow sprain
- Golfer’s elbow
- Tennis elbow
- Other issues or injuries to the normal anatomy of the elbow
- Hand and Wrist
-
We treat many common hand-related health conditions and offer state-of-the-art care for hands and wrists.
Trigger Finger
The tendons of the thumb and each of the fingers pass through a sheath on the palm side of the hand. Certain diseases and overuse activities can cause it to thicken. Eventually, the tendon becomes irritated and swells. Pain, catching and locking of the finger will occur. Early treatment consists of anti-inflammatory medication or cortisone injections. If these don’t provide relief, minimally invasive surgery is recommended.
Dupuytren's Contracture
This disorder is an abnormal thickening of tissues in the palm, resulting in nodules on the ligament, which, if severe enough, can cause an inability to straighten the fingers fully. No surgery is needed if the condition is mild and there is no functional loss. But if it interferes with the full use of the hand, surgery can improve function and prevent further deformity.
De Quervain's Tenosynovitis
Tendonitis around the thumb can be painful and disabling, making simple pinching and twisting almost impossible. Treatment consists of rest, medication and occasionally the use of a steroid injection. If these treatments do not provide relief over time, the tendons can be surgically released.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is a common problem resulting from pressure on the median nerve at the wrist. Symptoms, often worse at night, consist of numbness and pain in the wrist and fingers. Eventually, there is a loss of strength, fine motor control and sensation.
Early treatment consists of splinting and anti-inflammatory medication. If symptoms do not improve, an outpatient surgical procedure to relieve the pressure on the nerve is suggested.
- Fractures and Trauma
-
While many fractures result from high-force impact or stress, bone fractures can also occur due to certain medical conditions that weaken the bones, such as osteoporosis.
We treat bone fractures in multiple areas of the body:
Foot and Ankle
- Ankle fractures
- Heel fractures
- Lisfranc (midfoot) fracture
- Stress fractures of the foot and ankle
- Talus fractures
- Toe and forefoot fractures
Hip
- Hip and pelvis fractures
Knee and Leg
- Fractures of the proximal tibia
- Pediatric thighbone fracture
- Shinbone fractures
- Thighbone fracture
Shoulder, Arm and Elbow
- Broken arm
- Broken collarbone
- Elbow fractures
- Fracture of the shoulder blade
- Pediatric elbow and forearm fractures
- Radial head fractures
- Shoulder trauma
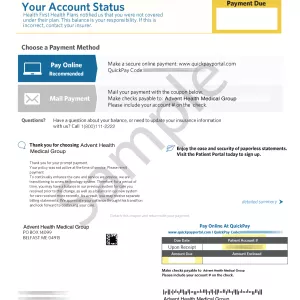
Safe, Secure Online Bill Pay
It's easy to pay your bill online. Access your account and make a payment for services at all AdventHealth locations in one place. For information about your bill, please call 303-552-3024.
Instructions for Our Surgical Patients
If you are having same-day surgery, you must have a ride home and someone to stay with you overnight.
Do not eat or drink after midnight the evening before your surgery, or your surgery will be canceled. You are allowed to take necessary medications with a sip of water.
All aspirin, anti-inflammatory medications, vitamins and supplements must be stopped seven days before surgery.
If you feel ill or have any questions, please call the office.
If you have a heart condition, you must be seen by your cardiologist for clearance.
A surgical assistant may be present during your surgery to provide the best possible outcome. This may or may not be a covered benefit with your insurance. Please be aware that if it is not covered by the insurance, in part or in full, the patient is ultimately responsible for any charges incurred.
All medication refill requests must be made through your pharmacy.
Global care covers you for 90 days following your surgery. During that 90-day time frame, you will not be assessed a charge for your office visits. X-rays, casts, injections and splints will be billed to your insurance. Most, but not all, insurances do not require you to pay a copay, coinsurance or deductible during your global period, but some do. If you have questions about whether your insurance carrier will charge you a separate copay, please contact your insurance directly.
Preparing mentally and physically for surgery is an important step toward healing and recovery.
Before surgery, your doctor will examine you to ensure you have no conditions that could interfere with the surgery or its outcome. Routine tests, such as blood tests and X-rays, are usually performed a week before any major surgery. Discuss any medications you are taking to see which ones you should stop before surgery.
If you are currently trying to lose weight, doing so before surgery can help decrease the stress on your new joint. However, it’s best not to diet during the month before your surgery.
Arrange for someone to help with everyday tasks like cooking, shopping and laundry. It also helps to put items you use often within easy reach, so you won't have to extend and bend as often. Removing loose rugs and taping down cords is also important to avoid tripping hazards.
If you are experiencing excessive bleeding or difficulty breathing, call 911 right away to get medical care.
Postoperative instructions will be reviewed with you before discharge, and you’ll receive a written copy. Please ask whether you can drive, drink alcohol or make decisions for 24 hours after surgery or while you’re taking pain medication.
At Home
Please follow your surgeon's instructions once you return home. We’ll call you the morning after surgery to follow up and answer your questions, but contact us if you experience problems or changes in your condition.
If you had surgery on your leg, knee, hand or elbow, keep it elevated and use ice as directed. This will help decrease swelling and pain.
Pain Medication
Take your pain medicine as directed. Begin the pain medicine when you start getting uncomfortable, but before you are in severe pain. If you wait to take your pain medication until the pain is severe, you will have more difficulty controlling the pain.
If you have issues with your medication, call us to discuss alternatives.
Infection
If you develop any signs or symptoms of infection, such as persistent fever over 101 degrees, redness, warmth, swelling or increased pain, please call our office.
Complete Postoperative Care
We strive to increase the quality of care we offer our patients. The Center at Lincoln was created as a bridge between surgery and home, allowing our patients independence while recovering in a world-class facility.
Answering Common Spine and Joint Questions
-
Q:Question: Why is arthroscopy necessary?
A:Answer:Diagnosing joint injuries and disease begins with a thorough medical history, physical examination and usually X-rays. Additional diagnostic tests like an MRI or CT scan may also be needed. A final diagnosis is made through the arthroscope, which may be more accurate than a diagnosis reached from open surgery or X-rays.
-
Q:Question: Which joints can be viewed with an arthroscope?
A:Answer:Although the inside of nearly all joints can be viewed with an arthroscope, six joints are most frequently examined with this instrument. These include the knee, shoulder, elbow, ankle, hip and wrist. As medical engineers make advances in electronic technology and orthopedic surgeons develop new techniques, other joints may be treated more frequently in the future.
-
Q:Question: What are the conditions that can be treated through arthroscopy?
A:Answer:Several disorders are treated with a combination of arthroscopic and standard surgery, including some problems associated with arthritis. Disease and injuries can also damage bones, cartilage, ligaments, muscles and tendons.
Some of the most frequent conditions found during arthroscopic examinations of joints are:
- Inflammation
- Synovitis: inflamed lining in the knee, shoulder, elbow, wrist or ankle
- Chronic and acute injuries
- Shoulders: rotator cuff tendon tears, impingement syndrome and recurrent dislocations
- Knees: cartilage tears, chondromalacia (wearing or injury of cartilage cushion) and ACL tears with instability
- Wrists: carpal tunnel syndrome
- Loose parts of bone or cartilage in the joint
-
Q:Question: What is the rotator cuff?
A:Answer:The rotator cuff is a band of muscles surrounding the joint that connects the upper arm to the shoulder blade. The rotator cuff is stiff enough to hold the joint together but is also flexible enough to allow the arm to reach and lift.
Rotator cuff injuries are common among baseball pitchers, tennis players and other athletes who frequently exert an overhand throwing or swinging motion. Non-athletes who frequently lift or reach, such as stacking cans on a high shelf, can also develop rotator cuff problems.
-
Q:Question: What causes shoulder problems?
A:Answer:Most shoulder problems are the result of overuse or traumatic injury. Athletes who play high-contact sports like hockey or football often have shoulder injuries. Frequent lifting and repetitive arm rotation can also cause wear and tear on the shoulder. Inflammatory diseases such as arthritis and bursitis may develop over time.
-
Q:Question: What are the types and causes of arthritis in the knee?
A:Answer:The usual type of arthritis is osteoarthritis or degenerative joint disease. It’s also known as wear-and-tear arthritis since the cartilage simply wears out.
When the cartilage wears away, bone rubs on bone, causing severe pain and disability. The most common reason for osteoarthritis is in our genes since the durability of each person’s cartilage is based on genetics.
Trauma can also lead to osteoarthritis. A bad fall or blow to the knee can injure the joint. If the injury does not heal properly, extra force may be placed on the joint, which, over time, can cause the cartilage to wear away.
Inflammatory arthritis is swelling and inflammation of the joint lining, causing a release of enzymes that soften and eventually destroy the cartilage. Rheumatoid arthritis, Lupus and psoriatic arthritis are inflammatory conditions.
Expert Orthopedic Care Near South Denver
AdventHealth Medical Group Orthopedics and Spine at Inverness AdventHealth Medical Group Orthopedics and Spine at Inverness
-
Hours Information:Monday8 am to 5 pmTuesday8 am to 5 pmWednesday8 am to 5 pmThursday8 am to 5 pmFriday8 am to 5 pmSaturdayClosedSundayClosed
-
Parking Information:Free parking available on site







